Early and regular eye screening is the best defence for diabetics against loss of vision
Several years ago, while volunteering as a consultant to teach local eye doctors for a charitable organisation in rural China, I was eager to share the strategies applied in healthcare in Singapore against the rise of diabetes mellitus, an increasingly common disease. I believed that our emphasis on public education, early screening and management of diabetes with a view to prevent and delay complications work well. To my fellow ophthalmologists in the Chinese hospitals, I recommended our methods of early and regular eye screening for detection of diabetes- associated eye diseases, such as cataracts, glaucoma and diabetic retinopathy, the latter being an eye disease that affects the retina, the receptors of light at the back of the eye.
For the far-flung corners of the land, I showed them examples of mobile eye screening services, on a bus, that several countries such as Britain and Singapore employ. It was my sincere wish that my suggestions would be heeded by the hospital I visited, as the cases of diabetic eye disease that I witnessed there were very advanced and some beyond hope of repair. And I counted my blessings of being both a provider and user of the Singapore medical system. Let’s refresh ourselves about diabetes and the importance to guard against it. Just two years ago, a single medical condition, diabetes mellitus, was flagged for the first time, to my knowledge, at the National Day Rally by Prime Minister Lee Hsien Loong, as a national priority that needed to be addressed.
Complications
A metabolic disease that affects the control of sugar in our bodies, diabetes can result in complications such as blindness, kidney failure and gangrene, consequently requiring amputations. It also makes diseases like heart attacks and strokes more common. One in nine adults aged 18-69 here suffer from it, and the figure increases in the older age group. Type II diabetes affects the majority of the sufferers especially those over 40 yet is highly preventable by lifestyle modification. It costs taxpayers S$1 billion a year, and the figure is expected to increase yearly.
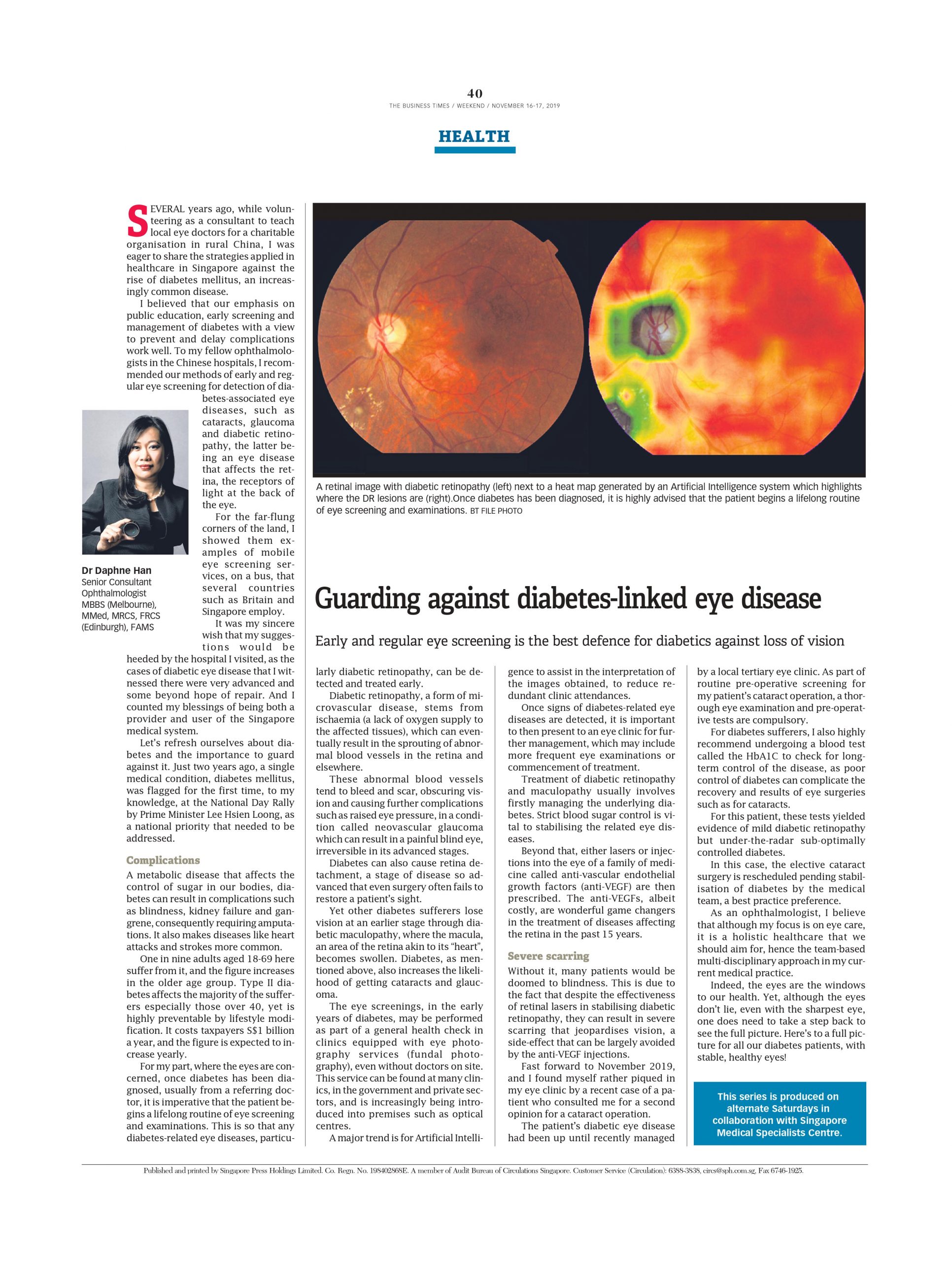
For my part, where the eyes are concerned, once diabetes has been diagnosed, usually from a referring doctor, it is imperative that the patient begins a lifelong routine of eye screening and examinations. This is so that any diabetes-related eye diseases, particularly diabetic retinopathy, can be detected and treated early. Diabetic retinopathy, a form of microvascular disease, stems from ischaemia (a lack of oxygen supply to the affected tissues), which can eventually result in the sprouting of abnormal blood vessels in the retina and elsewhere.
These abnormal blood vessels tend to bleed and scar, obscuring vision and causing further complications such as raised eye pressure, in a condition called neovascular glaucoma which can result in a painful blind eye, irreversible in its advanced stages. Diabetes can also cause retina detachment, a stage of disease so advanced that even surgery often fails to restore a patient’s sight. Yet other diabetes sufferers lose vision at an earlier stage through diabetic maculopathy, where the macula, an area of the retina akin to its “heart”, becomes swollen. Diabetes, as mentioned above, also increases the likelihood of getting cataracts and glaucoma.
The eye screenings, in the early years of diabetes, may be performed as part of a general health check in clinics equipped with eye photography services (fundal photography), even without doctors on site. This service can be found at many clinics, in the government and private sectors, and is increasingly being introduced into premises such as optical centres. A major trend is for Artificial Intelligence to assist in the interpretation of the images obtained, to reduce redundant clinic attendances.
Once signs of diabetes-related eye diseases are detected, it is important to then present to an eye clinic for further management, which may include more frequent eye examinations or commencement of treatment. Treatment of diabetic retinopathy and maculopathy usually involves firstly managing the underlying diabetes. Strict blood sugar control is vital to stabilising the related eye diseases. Beyond that, either lasers or injections into the eye of a family of medicine called anti-vascular endothelial growth factors (anti-VEGF) are then prescribed. The anti-VEGFs, albeit costly, are wonderful game changers in the treatment of diseases affecting the retina in the past 15 years.
Severe scarring
Without it, many patients would be doomed to blindness. This is due to the fact that despite the effectiveness of retinal lasers in stabilising diabetic retinopathy, they can result in severe scarring that jeopardises vision, a side-effect that can be largely avoided by the anti-VEGF injections. Fast forward to November 2019, and I found myself rather piqued in my eye clinic by a recent case of a patient who consulted me for a second opinion for a cataract operation. The patient’s diabetic eye disease had been up until recently managed by a local tertiary eye clinic. As part of routine pre-operative screening for my patient’s cataract operation, a thorough eye examination and pre-operative tests are compulsory.
For diabetes sufferers, I also highly recommend undergoing a blood test called the HbA1C to check for long-term control of the disease, as poor control of diabetes can complicate the recovery and results of eye surgeries such as for cataracts. For this patient, these tests yielded evidence of mild diabetic retinopathy but under-the-radar sub-optimally controlled diabetes. In this case, the elective cataract surgery is rescheduled pending stabilisation of diabetes by the medical team, a best practice preference.
As an ophthalmologist, I believe that although my focus is on eye care, it is a holistic healthcare that we should aim for, hence the team-based multi-disciplinary approach in my current medical practice. Indeed, the eyes are the windows to our health. Yet, although the eyes don’t lie, even with the sharpest eye, one does need to take a step back to see the full picture.
Here’s to a full picture for all our diabetes patients, with stable, healthy eyes!
Dr Daphne Han
Senior Consultant Ophthalmologist
MBBS (Melbourne), MMed, MRCS, FRCS (Edinburgh), FAMS
THE BUSINESS TIMES WEEKEND NOVEMBER 16 – 17, 2019